Generalized Anxiety Disorder: When Your Brain’s Alarm System Won’t Turn Off
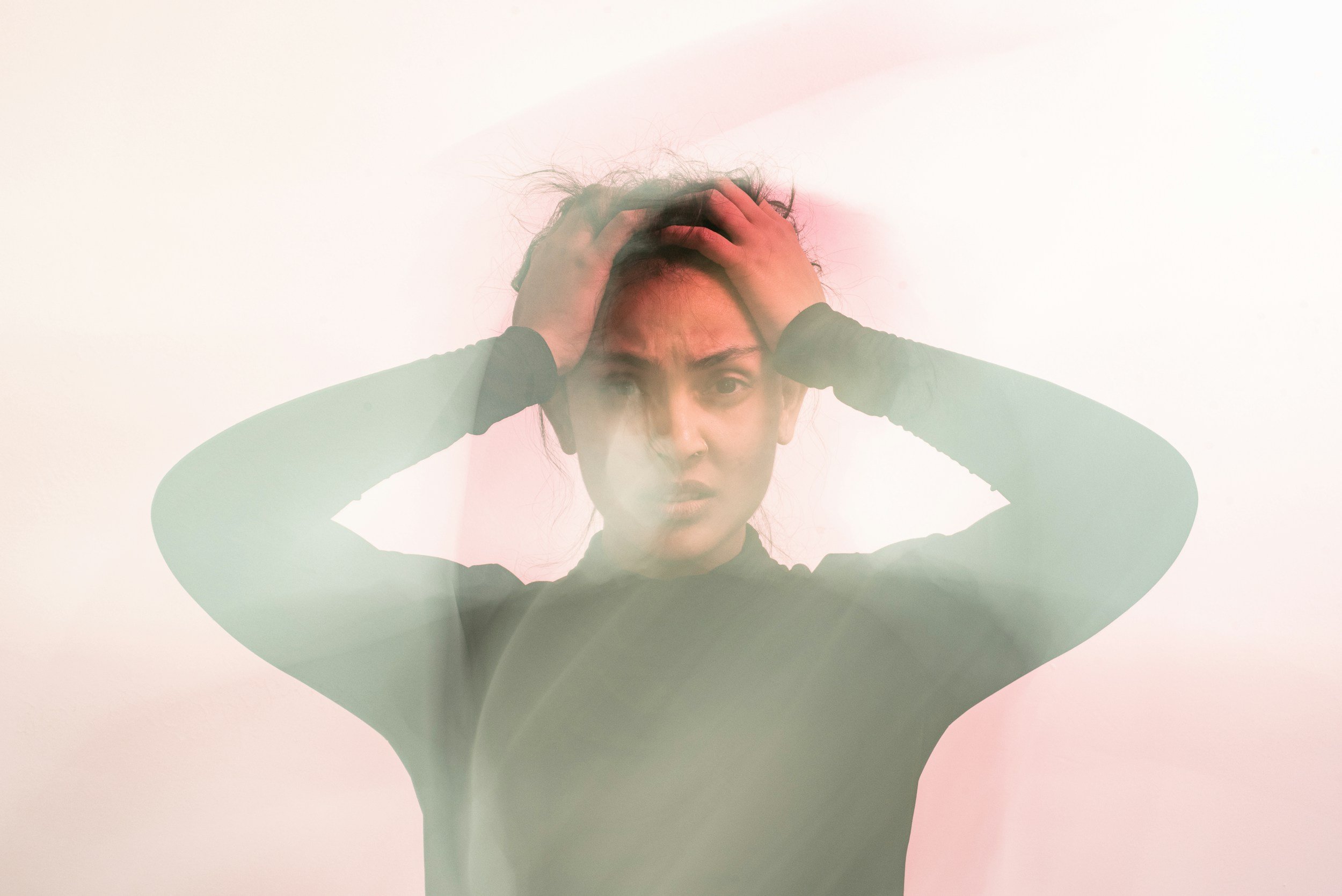
If you live with constant “what if” thoughts, a tight chest, restless sleep, and a sense that you can’t relax, even when life is going relatively well, you’re not alone. Sadly, anxiety is almost like a normal state of being in the U.S. It doesn’t have to be that way. So what is pathological anxiety versus normal stress? Generalized Anxiety Disorder (GAD) is a common and highly treatable condition. It’s more than periodic worry and everyday stress: it’s persistent, excessive worry that feels uncontrollable and starts to affect your mood, body, relationships, and daily functioning.
First, check out this fantastic YouTube video I found that goes over generalized anxiety disorder in great detail.
The Pathology: An Amygdala in Overdrive
One helpful way to understand GAD is through the amygdala: a small, almond-shaped structure in the brain involved in detecting threat and triggering fear responses.
In GAD, the amygdala can behave as if danger is everywhere, even when you’re safe. When the brain’s threat detector stays in a near-constant state of high alert, it can lead to:
Chronic psychological symptoms (persistent worry, fear, irritability)
Physical symptoms (muscle tension, fatigue, stomach upset, racing heart)
Functional impairment (difficulty concentrating, avoiding situations, disrupted sleep)
Over time, worry can become out of proportion to the actual situation and cause significant distress in daily activities—work, school, parenting, health decisions, social life, and even restful downtime.
How GAD Is Diagnosed
Generalized Anxiety Disorder has a clear diagnostic pattern. GAD involves:
Uncontrollable, excessive anxiety and worry across multiple areas of life, most days of the week for at least 6 months, along with at least three of the following symptoms:
Restlessness or feeling “on edge”
Fatigue or low energy
Impaired concentration or mind going blank
Muscle tension
Sleep disturbances (difficulty falling asleep, staying asleep, or non-restorative sleep)
In other words: it’s not only worry, it’s worry plus a sustained stress response that shows up in the body.
Important: Always Rule Out Medical and Substance-Related Causes
Before we label symptoms as anxiety, good clinical care includes evaluating whether something else could be driving them.
At Sweetgrass Psychiatry, we routinely consider and rule out contributors such as:
Thyroid dysfunction (especially hyperthyroidism, which can mimic anxiety)
Substance misuse or medication effects (including stimulants, excess caffeine, certain supplements, alcohol withdrawal, and other substances)
Hypoxia (low oxygen states that can produce panic-like symptoms, shortness of breath, and agitation)
Metabolic abnormalities (including problems that affect electrolytes, blood sugar, or systemic physiology)
This doesn’t mean anxiety “isn’t real.” It means we take symptoms seriously and make sure we’re treating the right root cause.
Psychological Symptoms of GAD
People with GAD often describe an internal experience like:
“My mind won’t shut off.”
“I know it’s irrational, but I can’t stop thinking about it.”
“I always feel like something is about to go wrong.”
Common psychological symptoms include:
Uncontrollable, excessive worry across several settings (health, family, work, finances, relationships, world events)
Fear and dread, often without a single identifiable trigger
Agitation, feeling “wired,” or unable to relax
Impatience or irritability (often from feeling chronically overwhelmed)
Impaired concentration (your brain is busy scanning for threats, leaving less bandwidth for focus)
Many people also develop patterns that temporarily reduce anxiety but reinforce it long-term, such as:
Phobias (fear of certain situations or bodily sensations)
Reassurance seeking (asking the same question repeatedly, checking repeatedly, needing constant confirmation)
Avoidance of anxiety-provoking situations (social plans, travel, phone calls, medical visits, difficult conversations)
These behaviors are understandable. They’re your brain’s attempt to find certainty and safety. But they can shrink your world over time.
Physiological Symptoms: The Sympathetic Nervous System at Work
GAD is not “just in your head.” Persistent worry can keep the sympathetic nervous system (your fight-or-flight response) activated. When your body is in that state too often, you may notice symptoms such as:
Common physical symptoms
Restlessness, an urge to move, difficulty sitting still
Muscle aches or chronic muscle tension (often neck, shoulders, jaw)
Clammy hands
Racing heartbeat or palpitations
Sweating
Shakiness
Extreme fatigue (from constant “activation” and poor sleep)
Throat and breathing sensations
Lump in the throat
Choking sensation
Hyperventilation or feeling short of breath
Digestive symptoms
Nausea
Vomiting
Diarrhea
Upset stomach or “knots” in the abdomen
Sleep disturbances
Sleep problems are especially common, often due to worry. This can include:
Difficulty falling asleep (mental “looping”)
Waking up frequently
Early morning awakening with worry
Non-restorative sleep even after adequate hours
When anxiety disrupts sleep, the next day’s anxiety is often worse—creating a cycle that can feel hard to break.
Treatment for GAD: A Practical, Evidence-Informed Approach
The good news: GAD is treatable. Many people experience meaningful improvement with a structured plan—often within weeks to months.
At Sweetgrass Psychiatry, we typically think of treatment in layers:
1) Psychotherapy (First-Line)
Therapy is often the foundation because it builds skills that last.
Two highly effective options include:
Cognitive Behavioral Therapy (CBT)
CBT helps you identify and change patterns like:
Catastrophizing (“If this happens, everything will fall apart”)
Overestimating risk and underestimating coping ability
Intolerance of uncertainty (“If I can’t be 100% sure, I can’t relax”)
Mindfulness-Based Stress Reduction (MBSR) / Mindfulness-Based Approaches
Mindfulness skills can help you:
Notice worry without getting pulled into it
Reduce physiological arousal
Build tolerance for uncertainty and uncomfortable sensations
Is psychotherapy necessary?
Not always—but it is often one of the most effective long-term strategies. Medication can reduce symptom intensity, but psychotherapy teaches the brain and body a new response pattern. For many people, the best outcomes come from combining therapy and medication.
2) Medications (Commonly SSRIs and SNRIs)
Medication can be especially helpful when anxiety is:
Persistent and impairing
Affecting sleep and concentration
Leading to avoidance or panic-like symptoms
Accompanied by depression
Two major medication classes used in GAD are:
SSRIs (Selective Serotonin Reuptake Inhibitors)
SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors)
These are not “instant anxiety pills.” They work gradually, often over several weeks, and are typically used as part of a broader treatment plan that includes behavioral strategies and lifestyle support.
3) Short-Acting Medications (Including Benzodiazepines)
Short-acting medications, such as benzodiazepines, may be used in limited situations for acute relief.
However, these require careful prescribing because they can carry risks, including:
Sedation and impaired coordination
Tolerance (needing higher doses over time)
Dependence and withdrawal
Interactions with alcohol and other sedating medications
In general, benzodiazepines are best viewed as a short-term, targeted tool, not a long-term solution.
When to Reach Out
Consider professional evaluation if anxiety is:
Present most days and hard to control
Affecting sleep, concentration, or relationships
Leading to avoidance or frequent reassurance seeking
Causing significant distress or interfering with daily life
And seek urgent help immediately if you experience thoughts of self-harm, feel unsafe, or are in crisis.
How Sweetgrass Psychiatry Can Help
At Sweetgrass Psychiatry, our approach to GAD is comprehensive and collaborative. We focus on:
Accurate diagnosis (and ruling out medical contributors like thyroid dysfunction, metabolic abnormalities, hypoxia, and substance-related causes)
Personalized treatment planning
Evidence-based therapy recommendations (CBT and mindfulness-based approaches)
Thoughtful medication management when appropriate
Helping you build sustainable, long-term resilience—not just symptom suppression
If you live in South Carolina and you’re ready to feel calmer, more focused, and more in control, we’re here to support you. Please fill out our new patient intake form online or you can call or text 843-800-1303 for more information and to determine if we are an appropriate fit for your needs.
This article is for educational purposes and is not a substitute for medical advice, diagnosis, or treatment. If you think you may have GAD or another mental health condition, please consult a qualified clinician.